Contents
Is Intermittent Fasting Considered Safe for Type 2 Diabetes?
Even though some studies show promising results, the safety of intermittent fasting for type 2 diabetes varies from study to study, and each case is unique.
As a result, diabetic patients are advised to consult with their physician before implementing an intermittent fasting regimen. This will ensure that the appropriate oversight is in place during the fasting period, tailored to their individual health needs.
Type 2 diabetes is a condition that occurs when your body doesn’t make enough insulin or does not respond to it appropriately. It results in blood sugar, or blood glucose, levels being too high.
The main difference between type 1 and type 2 diabetes is that type 1 diabetes is often a genetic condition that shows signs early in life, whereas type 2 is rather a lifestyle-induced condition that develops over time.
The most straightforward approach to managing type 2 diabetes is by adopting a healthy lifestyle. Moreover, studies have shown that following a healthy diet and engaging in regular exercise can significantly impact your blood sugar levels, which is an important aspect of managing diabetes.
A recent study of intermittent fasting demonstrated that a time-restricted eating method led to weight loss and improved glycemic control by reducing fasting glucose and insulin levels, decreasing leptin levels, and increasing adiponectin levels. However, additional research is required to distinguish the effects of intermittent fasting from those of weight loss alone.
Intermittent fasting can also be significant in reducing the risk of developing diabetes if you have been diagnosed with prediabetes.
Take a
1-minute quizand discover how much weight you can lose with DoFasting!
Is Intermittent Fasting Safe for Prediabetes?
Prediabetes is a health condition where blood sugar levels are higher than average but not high enough to be classified as type 2 diabetes. Without any lifestyle changes, prediabetes can progress to type 2 diabetes, which is why it is a condition that should be taken just as seriously as other forms of diabetes.
Prediabetes isn’t a permanent condition and can be reversed. The most important thing is to lead a healthy lifestyle and find ways to manage your blood sugar levels. One of the methods can be intermittent fasting, as it has been shown to impact people in the early stages of diabetes significantly.
For example, a 5-week study was conducted by the Pennington Biomedical Research Center to test the benefits of intermittent fasting for people with prediabetes.
During this randomized clinical trial, men with prediabetes were assigned to a 6-hour feeding period regimen, while the control group followed a 12-hour feeding period regimen.
After five weeks, the results were compared, and scientists noticed a significant increase in insulin sensitivity, improved blood pressure, and improved cell responsiveness, as well as a decrease in appetite for men who were in the intermittent fasting group.
While intermittent fasting is generally considered safe for people with prediabetes, it’s highly recommended to consult a healthcare professional before starting an intermittent fasting plan.
Additionally, intermittent fasting may not be suitable for certain groups of people, such as those with eating disorders, children and teenagers under the age of 18, and pregnant women.
Now, let’s move on to type 1 diabetes.
Is Intermittent Fasting Considered Safe for Type 1 Diabetes?
Type 1 diabetes is a condition when your body doesn’t make or makes very little of the hormone insulin, which makes blood sugar levels too high. The main difference from other types of diabetes is that type 1 diabetes is a genetic condition less related to your lifestyle. Type 1 diabetes is more likely to occur in the early stages of life. That’s why it’s also often called “juvenile diabetes.”
When it comes to intermittent fasting for type 1 diabetes, while initial studies show promising effects, it is currently advised against by various diabetes organizations, such as the American Diabetes Association. This is because fasting is believed to increase the risk of hypoglycemia and hyperglycemia, both serious conditions for people with type 1 diabetes.
If you do decide to try fasting with type 1 diabetes, it’s important to discuss glycemic control, medication doses, low blood sugar management, and other medication adjustments with a medical professional. This is to ensure that the risks are minimized and that you are able to manage your condition while fasting safely.
4 Benefits of Intermittent Fasting for Diabetes
Intermittent fasting isn’t a diet and instead, a time-restricted eating pattern that’s mostly known for helping people to lose weight. While it’s true, the benefits extend beyond weight loss.
1. Weight loss
The most straightforward way that intermittent fasting can help you lose weight is by reducing your calorie intake. Depending on the intermittent fasting plan you choose (such as 12:12, 14:10, 16:8, 18:6, 20:4, etc.), you’ll refrain from eating for a certain time period until your eating window opens.
Also, intermittent fasting can boost your metabolism. When you fast, for example, your nervous system releases norepinephrine into your fat cells, causing them to break down body fat into three fatty acids that may be used for energy.
Intermittent fasting can effectively reduce body weight, which can, in turn, lower the risk of diabetes complications such as heart disease and stroke. A study by Hormone and Metabolic Research has shown that losing weight can also reduce insulin resistance in type 2 diabetes.
For those with type 2 diabetes, losing approximately 5% of their weight can offer significant health benefits and, in some cases, even put diabetes into remission.
Although type 1 diabetes is not related to body mass, losing excess weight can still reduce the risk of complications and may lead to the need for fewer insulin injections. For those with prediabetes, losing weight, mainly if they are overweight, can decrease the risk of developing type 2 diabetes.
2. Glucose metabolism
During glucose metabolism, processes like glycolysis, gluconeogenesis, glycogenolysis, and glycogenesis take place. This is the process by which our cells receive energy from glucose.
After we eat carbohydrates, they are broken down into simple sugars: fructose, which comes from fruits and honey; galactose, which comes from dairy products; and glucose, which comes from grains, fruits, and vegetables. Apart from fruits and vegetables, there are a few other sources of fructose, such as honey and some processed meals.
In the process of glucose metabolism, these sugars are converted to glucose, which is the primary fuel source for our cells. When glucose levels in the bloodstream rise, the pancreas releases insulin, which helps glucose enter the cells and be used for energy.
The problem occurs when the body is unable to produce enough insulin (Type 1 diabetes), or when the cells don’t respond to insulin properly (Type 2 diabetes and prediabetes). This leads to a situation where our cells can’t properly absorb glucose from the bloodstream, and our blood sugar levels remain high.
Without enough insulin or proper insulin function, our cells are unable to receive the nutrition they need, and our blood sugar levels remain elevated with excess glucose that’s unable to enter the cells. This can lead to a range of symptoms and complications associated with diabetes.
Intermittent fasting can help improve glucose metabolism in people with diabetes by reducing insulin resistance and improving insulin sensitivity. During fasting periods, your body uses stored fats instead of glucose as the main source of energy.
This can help reduce glucose levels in the bloodstream and improve insulin sensitivity.
Additionally, during fasting periods, the body’s glucose levels decrease, causing the pancreas to release glucagon, which promotes the breakdown of glycogen in the liver and helps to maintain blood glucose levels.
3. Insulin resistance
Insulin resistance is a condition in which the body doesn’t respond properly to insulin, a hormone essential for regulating blood sugar levels. This can occur in anyone, regardless of whether they have diabetes, and can be either temporary or chronic.
The two main factors that can contribute to insulin resistance are excess body fat, particularly abdominal fat, and physical inactivity. Other factors, such as genetics, age, and certain medical conditions, can also play a role in the development of insulin resistance.
Insulin resistance is usually experienced by people with prediabetes and type 2 diabetes and can sometimes occur in people with type 1 diabetes.
Intermittent fasting has been found in studies to improve insulin resistance. In fact, prolonging the time between meals allows your body to reach energy storage areas. Insulin resistance increases when your stored energy is routinely exhausted.
4. Blood pressure management
High blood pressure is a risk factor for heart disease. It can damage your arteries by making them less elastic, decreasing blood and oxygen flow to your heart.
People with diabetes are at an increased risk of high blood pressure, which can further increase the risk of heart attack or stroke. However, there are many ways to manage blood pressure and reduce this risk. Medication is one option, but lifestyle changes such as a healthy diet and regular exercise can also be very beneficial.
In addition to diet and exercise, research suggests that fasting may also help lower blood pressure, reduce cholesterol levels, improve blood sugar control, and support weight loss in people with diabetes.
Intermittent fasting can also reduce inflammation, which can be a contributing factor to high blood pressure.
It’s important to note that blood pressure control is important for all individuals with diabetes, regardless of type. Regular check-ups and monitoring of blood pressure levels are crucial for identifying and addressing any potential issues. If blood pressure is consistently elevated, it’s important to work with a healthcare provider to develop a treatment plan that may include medication, lifestyle changes, or a combination of both.
Take a
1-minute quizand discover how much weight you can lose with DoFasting!
Can Intermittent Fasting Reverse Diabetes?
Type 2 diabetes cannot be completely reversed, but the symptoms and complications of the disease can be significantly improved with appropriate management. Intermittent fasting is a promising approach, which has been shown to address some of the underlying causes of insulin resistance and improve blood sugar control.
It’s important to note that intermittent fasting is most relevant for people with type 2 diabetes, which is typically associated with lifestyle factors such as excess body weight and physical inactivity. Type 1 diabetes, on the other hand, is an autoimmune condition that cannot be prevented or cured.
Multiple studies have demonstrated the effectiveness of intermittent fasting for improving insulin resistance and reducing the need for medication in people with type 2 diabetes. However, it’s important to work with a healthcare provider to determine the most appropriate treatment plan, which may include medication, lifestyle changes, or a combination of both.
Types of Intermittent Fasting for Diabetes
There are several types of intermittent fasting for diabetes, each with its own guidelines.
The 5:2 diet
The 5:2 is a unique approach in which you follow your regular diet for 5 days and then restrict your calorie intake for the remaining two days. On these two days, you can consume no more than 500-600 calories per day.
During the non-fasting days, you should eat a healthy and well-balanced diet to achieve the best results.
The fasting method is quite flexible and easy to follow, and you can plan your fasting days however you want. Nonetheless, taking one non-fasting day in between is strongly recommended.
A study by the University of South Australia found that the 5:2 diet results in weight loss and improves blood glucose control.
Time-restricted diet
Time-restricted eating involves focusing on timing rather than calorie intake. You eat during specific hours and then refrain from consuming anything for a set amount of time, with the fasting periods being longer than a normal overnight fast of 8-12 hours.
There are various schedules of varying difficulty. For example, a 14:10 schedule means a 10-hour window for eating and 14 hours of fasting, while a 16:8 schedule provides 8 hours for eating and the remaining 16 hours for fasting.
During the eating window, you can consume whatever you want, but during fasting, only non-caloric beverages like water, tea, and black coffee are allowed.
Time-restricted eating has been shown to have many positive effects on people with diabetes, including improved insulin sensitivity, reduced body weight, and improved cholesterol levels. Furthermore, periodic fasting may be easier to adjust to and have a lower likelihood of side effects, such as dizziness, compared to periodic eating.
Fasting-mimicking diet
The fasting-mimicking diet is an alternative way to achieve a fasting state. Unlike traditional fasting, this type of fasting allows the consumption of certain foods and beverages in limited amounts.
Currently, there is only one clinically tested fasting-mimicking diet on the market, known as ProLon. This program lasts for five days and involves carbohydrate restriction and a high-fat food combination, with daily food intake typically ranging from 700 to 1,100 calories.
Speaking of fasting-mimicking diet and diabetes, a study conducted by Science Translational Medicine found that three cycles of ProLon resulted in reduced body weight, improved blood pressure, and beneficial effects on total body fat. This suggests that the fasting-mimicking diet may be an effective way for people with diabetes to manage their weight and improve their overall health.
However, it is important to note that more research is needed to fully understand the long-term effects of this type of diet on diabetes management.
Tips for Intermittent Fasting With Diabetes
To make the most out of intermittent fasting with diabetes, there are various steps you can take.
Talk to your doctor
Since each case of diabetes is unique, it’s advisable to consult with your healthcare specialist before starting an intermittent fasting routine. This can help you choose the right fasting type.
Additionally, your doctor can adjust your medication and insulin dosages accordingly. Changes in your diet may affect your blood sugar levels, which may necessitate adjustments to your diabetes treatment.
Test your blood sugar frequently
One of the risk of fasting with diabetes is the fact that it causes a significant drop in blood sugar levels. When you fast for a prolonged period of time, your body starts using stored glucose for energy. This might cause your blood sugar levels to drop even more, especially if you are on diabetes medication.
This can also lead to hypoglycemia, which is a state when your blood sugar levels drop too low. The most common symptoms of hypoglycemia include shaking, sweating, disorientation, and dizziness.
Hence, it’s important to regularly check your blood sugar levels when fasting to avoid these symptoms.
The foods you eat also matter
Food has a big influence on blood sugar levels, especially if you have diabetes. Eating high-carbohydrate meals can induce a surge in blood sugar levels, which can lead to difficulties when fasting. To avoid this, it’s critical to eat a well-balanced diet rich in nutrient-dense foods.
As a result, try to incorporate vegetables which are known to regulate blood sugar levels by being high in fiber. Protein is also essential as it can help you feel full and satisfied, which can prevent overeating.
Find a plan that works for you
Before starting any fasting routine, it’s crucial to find a plan that works for you. This involves determining how many hours you can comfortably go without eating and still feel good. It’s also essential to consider your overall health and medical history when selecting a fasting plan.
If you’re new to fasting, the fasting-mimicking diet may be a good starting point. This type of diet allows you to eat a limited number of calories while still reaping the benefits of fasting. It can be an excellent way to ease into a more extended fast or to maintain a healthy eating pattern.
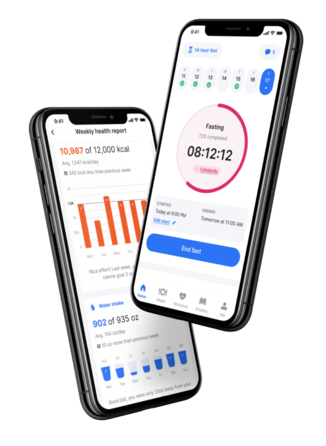
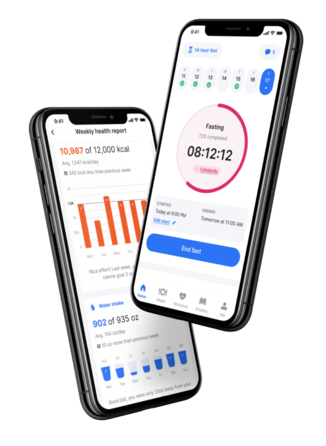
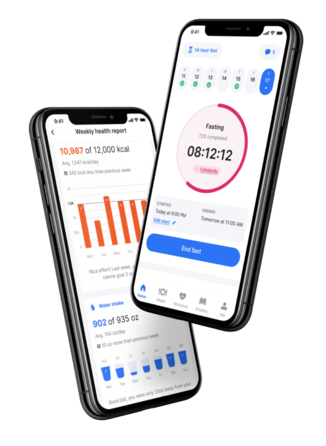
There are several tools available to assist you in determining the best fasting plan for you, including the DoFasting app. This app is designed to help users in determining the appropriate fasting plan for them based on their goals, preferences, and personal information.
Take a
1-minute quizand discover how much weight you can lose with DoFasting!
Intermittent Fasting for Diabetes: Key Takeaways
Intermittent fasting can offer several benefits for people with diabetes, including improved insulin sensitivity, reduced glucose levels, weight loss, and easier blood sugar management. These benefits can lead to a healthier and happier life, but it’s essential to approach fasting with caution and consideration.
Before starting an intermittent fasting program, you should consult with a medical professional to ensure that it is safe and appropriate for you. The medical professional can help you recognize the risks and benefits of fasting and develop an approach that is tailored to your specific needs.
See how DoFasting will improve your life
Find out what works for you with this 60-sec quiz approved by our experts and get your personal revolutionary fasting assistant.
Start the Quiz
This is an evidence-based article that includes scientific citations. DoFasting’s professional writers and editors prepared the content, which a team of medical experts verified to be accurate.